Their baby died. Then they got the $58K hospital bill.
Their baby spent the last four days of her life in the ICU.
Weeks later, her grieving parents received the $58,000 bill for the ICU stay, which was not covered by their insurance provider, Anthem Blue Cross Blue Shield.

A doctor was forced to scrub out of surgery to justify the procedure to UnitedHealth Care
Dr Elizabeth Potter shared her story in a video that has since gone viral. More and more frequently, it is insurers, rather than doctors, deciding treatments for patients.

Blue Cross and Blue Shield denied covering the cost of one metro woman’s life-saving medicine, leaving her with an over $8,000 monthly bill.
As of today, she is still left without the meds she needs. She posted her story, and it went viral, she says she refuses to be silent not for her but for the people who have no one to fight for them.
INSURERS PUT PROFITS OVER PATIENTS
RECORD BREAKING REVENUES
The United States is the only major developed country not to guarantee healthcare for all, spending nearly twice as much per capita as compared to other nations. And yet, we have among the worst health outcomes, with an estimated 68,000 Americans dying annually from lack of access to health services.
As reported in Mother Jones, according to the Kaiser Foundation: “Average annual out-of-pocket medical costs, adjusted for inflation, have more than doubled since 1970, to $1,425 per person in 2022. And remember that healthy people don't pay nearly so much. It's the sicker folks who face the high out-of-pocket costs. In fact, roughly a quarter of insured people with certain chronic health conditions said they were skipping doses of medications their doctors prescribed, or hadn't gotten prescriptions filled, because of the cost.”
While the average American struggles, there is one group that is doing very well: corporate executives.
Even as millions of Americans struggle with medical debt, for the insurance industry, healthcare has never been more profitable. Between 2013 and 2023, insurers increased their revenues by 345.8%, their profits skyrocketing by billions.
INSURERS PRIORITIZE COST OVER CARE
MORE DENIALS MEAN MORE DOLLARS
The system is designed to return profits, not to provide care. Claims are often processed by medical benefits management companies. The biggest of these companies is EviCore, which uses an AI algorithm some users call “the dial.” This algorithm can be dialed up to increase denial rates, which in turn means increased profit for executives and shareholders.
AI processing has sometimes resulted in absurd denials. As reported in The Washington Post, one insurer’s letter was sent directly to a newborn child denying coverage for his fourth day in a neonatal intensive-care unit. “You are drinking from a bottle,” the denial notification said, and “you are breathing on your own.”
For the pursuit of profit, claims are denied even when the insurance company’s denial is in violation of the law.
A Michigan law requires coverage of cancer drugs. 50-year-old Forrest VanPatten had a hyperaggressive form of lymphoma. He was a good candidate for treatment, with a fierce drive to stay alive for his wife of 25 years and their grown kids. He and his family hoped that treatment would save his life. Instead, his insurance company refused to approve it.
A ProPublica investigative report found that across the country, health insurers are flouting state laws like the one in Michigan. State legislators thought they’d solved the problem by passing hundreds of laws spelling out exactly what had to be covered. But companies have continued to dodge bills for treatments, even as industry profits have risen. ProPublica identified dozens of cases in which plans refused to pay for high-stakes treatments or procedures — from emergency surgeries to mammograms — even though laws require insurers to cover them.
Patients’ needs weren’t part of the equation, VanPatten’s health insurance company’s chief medical officer told ProPublica. “It was, ‘This is really expensive, how do we stop payment?’”
INSURERS BREAK THE LAW
LITTLE TO NO LEGAL REPERCUSSIONS
Regulators never intervened when VanPatten’s insurer failed to provide coverage for his cancer treatments, even though the law should have protected him. He died without knowing his treatment should have been covered. An investigation by ProPublica found that even when states enact laws to protect patients, state regulatory agencies lack the resources necessary for enforcement. When agencies do step in, it's usually because a policyholder files a complaint, but one study found this happens less than 1% of the time. Patients often do not know which regulatory agency to contact or how to navigate the complex bureaucracy.
For insurance corporations, breaking the law can be immensely profitable. In one egregious recent example, UnitedHealth Group, along with CVS and Cigna, have been caught charging patients a markup for key life-saving drugs that could easily exceed their cost by a factor of ten or more, according to findings from the Federal Trade Commission. These corporations have raked in an extra $7.3 billion by price gouging.
A CLEAR CASE OF CORPORATE FRAUD
The Department of Justice is investigating UnitedHealth following allegations that the company profited off false diagnoses. Medicare Advantage, which is run by private insurers, covers nearly half of the 68 million Americans on Medicare. Insurers receive payment per patient but they receive more for patients with complex health conditions. Reportedly, UnitedHealth added diagnoses to patients’ records for conditions those patients were never actually treated for, fraudulently collecting an extra 8.7 billion dollars.
THE DOJ INVESTIGATES UNITEDHEALTH
INSURERS THREATEN WHISTLEBLOWERS
INSURANCE COMPANIES ARE QUICK TO SILENCE CRITICISMS
After Dr. Elizabeth Potter was forced to scrub out of surgery in order to call UnitedHealth to justify a patient’s hospital stay, she posted a video about the incident. "I had to scrub out mid-surgery to call United, only to find that the person on the line didn't even have access to the patient's full medical information, despite the procedure already being pre-approved," Potter stated. "It's beyond frustrating and, frankly, unacceptable. Patients and providers deserve better than this. We should be focused on care, not bureaucracy.”
The video went viral.
In response to Dr. Potter’s viral video, UnitedHealth swiftly retaliated, hiring a prominent defamation law firm to send a 7-page letter demanding Potter post a public apology and contact Newsweek and other media outlets recanting her claims. Potter is standing firm and urges other physicians not to succumb to silencing or bullying. Her channel remains active, and she has recently posted another video about a patient whose hospital stay was denied.
UNITEDHEALTH SENT A 7-PAGE LETTER THREATENING LEGAL REPERCUSSIONS


Dr. Potter is not the first to have gone viral for speaking up about insurance denials. A post by Dr. Zachary Levy garnered widespread attention after his patient’s hospitalization was deemed “not medically necessary” by UnitedHealth.
In a post that was viewed more than 13 million times before it was removed, Dr. Levy noted that his patient, who was in heart failure, in a coma, and on a ventilator, had her claim denied because UnitedHealth insisted that her care in the hospital had not been proven to be "medically necessary."
Levy's account on X was removed and later restored, though the post about UnitedHealthCare is not longer accessible.
AMERICANS ARE DROWNING IN DEBT
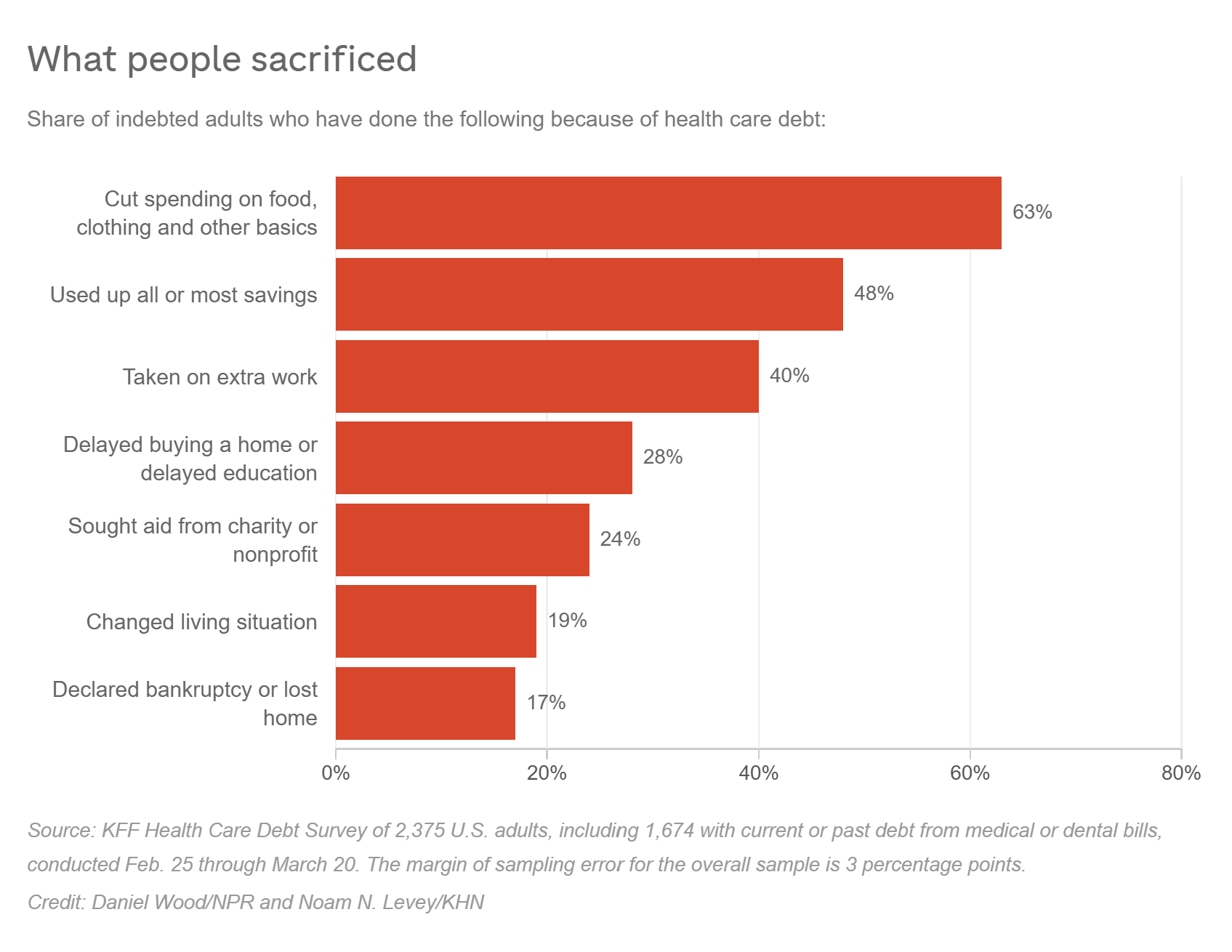
FAMILIES FORGO BASIC NECESSITIES DUE TO HEALTHCARE DEBT
Even as millions of Americans struggle with medical debt, for the insurance industry, healthcare has never been more profitable. Between 2013 and 2023, insurers increased their revenues by 345.8%, their profit increasing by billions.
Meanwhile, sick and struggling to pay, 100 million people in the U.S. live with medical debt. A quarter of adults with health care debt owe more than $5,000. And about 1 in 5 with any amount of debt said they don't expect to ever pay it off. The burden is forcing families to cut spending on food and other essentials, a poll by KFF found.
According to a 2019 article, roughly 250,000 campaigns for dealing with health care costs are set up annually on GoFundMe, and one-third of all donations made through the site help people pay for medical care.
More recently Ari Romio, a spokesperson for GoFundMe, stated that “medical expenses” is still the most common category of fundraiser, and in fact, because sometimes people put medical expenses under other categories (travel, for example, for medical care out of state), the number of GoFundMe campaigns dedicated to medical expenses may actually be higher.

When Jenn Coffey, 53, developed CRPS (complex regional pain syndrome), the monthly infusions cost her $5,000. UHC paid $1.22 towards one of the payments.
Due to repeated denials, Coffey, a former EMT, has been forced to sell her belongings and raise money on GoFundMe to cover her medical costs.

Amanda Boley was flown to the hospital after emergency responders found her without a pulse. Her insurance refused to cover the cost.
Anthem insurance informed her that the air ambulance that saved her life would have required her to call for pre-approval (despite her heart being stopped). She was left with a $64,998 bill.
Vivian Gonzales’s father had cancer. His doctor recommended an MRI and chemotherapy. His insurance caused delay after delay.
He died. “I spent so much time on the phone, writing letters, faxing… that I didn’t get to spend that time with my father,” she recalls.